The Complete Guide to Dental Implants
Published
20 June 2025 | 30 min read
Published
20 June 2025 | 30 min readArticle Summary
Everything You Need to Know about Dental Implants for a Healthy Smile
If you’re thinking about replacing missing teeth, dental implants are one of the most trusted and long-lasting solutions available today.
Dental implants offer stability, function, and a natural look that can improve your ability to eat, speak, and smile with confidence.
With advances in dental techniques, the process is now more predictable and accessible than ever before.

In our comprehensive guide, we will help you understand what dental implants are, how they work, and what you can expect throughout the process.
Whether you are missing one tooth or several, this guide covers everything from the benefits and different types of dental implants to potential risks, costs and how to care for your new smile.
Key Takeaways
- Dental implants restore function and appearance after tooth loss.
- There are several types and steps involved, each with unique benefits.
- Proper care keeps implants safe, healthy, and long-lasting.
What Are Dental Implants?

Dental implants are an important option for people who have lost teeth and want a strong, lasting solution.
They act as artificial roots for replacement teeth, helping us eat, speak, and smile with confidence.
Definition and Purpose
Dental implants are small metal posts, usually made of titanium, that dentists surgically place into the jawbone.
These posts act as artificial tooth roots, giving a secure base for attaching artificial teeth like crowns, bridges, or dentures.
The main purpose is to replace missing teeth in a way that feels and works much like natural teeth.
Implants help us chew food properly, speak clearly, and maintain the shape of our face and jaw.
Unlike removable dentures, implants are fixed in place and don’t slip or move around.
This makes them much more comfortable during daily activities.
Implants also help prevent bone loss in the jaw, which can happen when teeth are missing for a long time.
How Dental Implants Work
Dental implants rely on a process called osseointegration.
After the titanium implant is placed in the jawbone, the bone starts to grow around it.
This helps anchor the implant firmly, almost like how natural tooth roots are attached to the jaw.
The step-by-step process includes:
- Placing the implant post into the bone.
- Waiting several weeks for the bone to bond with the implant.
- Attaching a small connector called an abutment.
- Putting the artificial tooth, such as a crown, on top.
This creates a foundation for a prosthetic tooth replacement that is strong, stable, and natural-looking.
Because the implant fuses with our bone, it gives better support than traditional dentures or bridges.
History of Dental Implants
The idea of replacing missing teeth is very old.
Early versions of dental implants date back thousands of years.
Ancient civilisations sometimes used shells, pieces of metal, or carved stones as tooth replacements.
Modern dental implants began in the 20th century.
A key development was the discovery of osseointegration by Swedish scientist Per-Ingvar Brånemark in the 1950s.
He found that titanium could bond firmly with bone, which led to successful tooth implants.
Since then, dental implants have continued to improve.
Today, they are seen as a safe and reliable way to replace missing teeth, helping millions of people achieve better oral health and function.
Benefits of Dental Implants

Dental implants offer specific advantages that set them apart from other tooth replacement options.
These benefits include a more natural look, support for long-term oral health, lasting results, and improved daily comfort.
Natural Appearance and Comfort
Dental implants are designed to closely match the look of our natural teeth.
The crown, which sits on top of the implant, is custom-crafted to blend in with the colour, shape, and size of our existing teeth.
This helps our smile appear more natural and less noticeable than dentures or bridges.
Implants are anchored firmly in the jawbone.
Because of this, they do not slip or shift when we eat or talk.
The secure fit means we can enjoy favourite foods and speak clearly without worry.
Another important point is that dental implants feel comfortable in the mouth.
There are no bulky parts or special adhesives needed.
Most people adjust quickly and cannot feel a difference between the implant and their natural teeth.
We can brush and floss them just like our own teeth, making daily care simple and natural.
Improved Oral Health
When we lose a tooth, the gap it leaves can cause several issues for our oral health.
A major benefit of dental implants is that they help support the health of our jawbone by providing the stimulation that natural teeth roots give.
This reduces the risk of bone loss, which can happen with conventional dentures.
Unlike bridges, implants do not require us to grind down healthy teeth to support the replacement.
Our remaining natural teeth are left untouched, which keeps them stronger and healthier.
This also reduces the risk of decay or damage to those neighbouring teeth.
We can maintain a normal oral care routine with implants.
It is easy to clean between teeth and gums, lowering the chance of gum disease compared to some other tooth replacement options.
Details on these benefits can be found at OpenDent’s dental implant guide.
Long-Term Advantages
Dental implants are considered a permanent solution for missing teeth.
With proper care, they can last many years, often decades.
This is a key advantage over dentures and bridges, which typically need more frequent replacement or adjustment.
The materials used, like titanium for the post and durable ceramics for the crown, are strong and resist damage from normal biting and chewing.
This protects our investment in oral health.
Because implants preserve jawbone and gum health, they also help maintain the structure of our face over time.
This prevents the sunken appearance that can develop when bone is lost in areas missing teeth.
Implants rarely require the maintenance that some removable options do.
There are no extra appointments for relining or adhesives, which saves us time and hassle over the years.
Quality of Life Improvements
One of the biggest benefits of dental implants is how much they can improve our quality of life.
Eating with confidence, smiling without embarrassment, and being able to speak without worry are daily comforts that matter.
Implants allow us to eat a full range of foods, including crunchy fruits, vegetables, and chewy bread, without concern about slipping or pain.
This helps us keep a balanced diet and enjoy meals with family or friends.
Speech is often clearer with implants compared to dentures, which can shift and affect how we pronounce words.
We can express ourselves freely and naturally.
For many, there is also a psychological lift.
Our self-esteem improves when we are not self-conscious about missing teeth or removable dental work.
Dental Implant Components

Dental implants work by replacing the entire structure of a missing tooth.
To do this, they use several key parts that each serve a unique function in giving us a stable and long-lasting solution.
Titanium Post
The titanium post acts as the artificial tooth root and is the first part placed during the dental implant procedure.
We use titanium because it is strong, lightweight, and highly compatible with our body, reducing the risk of rejection or reaction.
This metal also allows the bone to grow around the post through a process called osseointegration, which helps keep the implant stable and secure.
Once placed in the jawbone, the titanium post becomes a permanent base for other components.
Over a period of a few months, the bone fuses directly to the titanium.
This connection makes the post a solid foundation for supporting chewing and normal mouth function.
Most modern implants use a threaded design which provides even more strength and stability.
A table showing titanium post features:
| Feature | Benefit |
|---|---|
| Made of titanium | Safe and durable |
| Threaded design | Extra stability |
| Osseointegration | Strong bone bond |
Find a clear breakdown of posts and their roles in dental implants at this dental implant components guide.
Abutment
The abutment is a small connector that joins the titanium post to the dental crown.
We fit the abutment after the titanium post has fully integrated with the bone.
Its main job is to hold the crown in place and keep it secure under normal bite pressure.
Abutments are usually made of titanium, zirconia, or stainless steel.
The choice depends on the location in the mouth and individual needs.
The abutment sits above the gum line, allowing us to attach the visible part of the replacement tooth while also protecting the underlying post from bacteria and infection.
Some abutments are angled to fit specific situations, giving better results for our smile and bite.
Properly selecting and placing the abutment is important for long-term success of the dental implant.
For more on abutment designs, see details at this in-depth exploration of implant parts.
Dental Crown
The dental crown is the visible artificial tooth that sits on top of the abutment.
We craft the crown to match the shape, size, and colour of our natural teeth.
This makes the final result look and feel as close to a real tooth as possible.
Crowns are often made from porcelain, ceramic, or a combination of materials for strength and a natural appearance.
Once the crown is fitted, it covers the abutment completely and becomes the surface we use for chewing.
A well-made permanent crown will withstand years of daily use.
Crowns also play a vital role in restoring our confidence and allowing us to eat, speak, and smile without worry.
For a complete look at crowns and their placement, read the complete guide to dental implant parts.
Types of Dental Implants
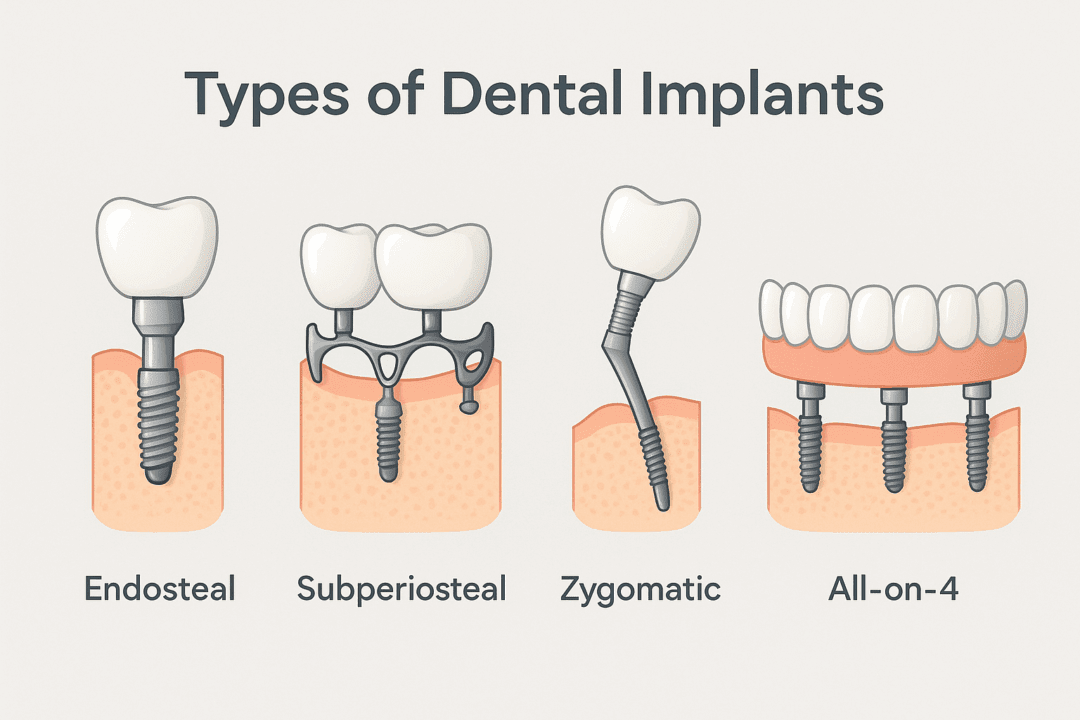
Dental implants are available in several main types, and the choice depends largely on the patient’s jawbone, health, and specific tooth replacement needs.
Each type has its own design and method for fitting into the jaw, with distinct benefits and uses.
Endosteal Implants
Endosteal implants are the most commonly used type. These implants are shaped like small screws, cylinders, or blades and are surgically placed directly into the jawbone.
We recommend endosteal implants to patients with a healthy, dense jawbone, as proper bone support is essential for success. Each endosteal implant acts as a root to support a single tooth implant, a dental bridge, or even dentures.
The process involves two main steps—first the implant post is placed, then after healing, a crown or artificial tooth is attached. Endosteal implants offer great stability and function almost like natural teeth.
They are effective for replacing one or multiple teeth. In most cases, they have a high success rate and can last for many years with good oral hygiene.
Learn more about endosteal implants and their uses.
Key facts:
- Placed in the jawbone
- Suitable for healthy bone
- Supports single or multiple tooth implants
Subperiosteal Implants
Subperiosteal implants are less common but useful for patients who do not have enough healthy jawbone for endosteal implants and who are unable or unwilling to undergo bone grafting. These implants rest on top of the jawbone but under the gum tissue, rather than being fixed into the bone itself.
A metal framework is designed and placed under the gums, with posts attached through the gums to hold the artificial teeth. For some patients with significant bone loss, this is a practical option when other types are not recommended.
Subperiosteal implants can often support several replacement teeth at once. They offer an alternative for those who have had extensive bone loss.
More information about subperiosteal implants and how they work.
Key facts:
- Sits above the jawbone, under the gum
- Ideal for those with insufficient bone
- Can support multiple artificial teeth
Candidacy for Dental Implants
Dental implants are a popular way to replace missing teeth, but not everyone qualifies for this procedure. Our overall oral health, jawbone strength, and planning with a dental professional are all important factors.
Assessing Bone Density and Jawbone Health
Successful dental implants rely on a healthy and dense jawbone. The implant post is inserted into the bone, so we must have enough bone to support it and keep it stable.
If we have had missing teeth for a long time, our jawbone may have started to shrink. Bone loss can also happen due to gum disease or injury.
Dentists often use X-rays or CT scans to check our bone density and jaw shape. For those with low bone density, bone grafting procedures might be suggested to help rebuild the jawbone.
Implants do more than replace teeth—they also help with bone preservation by stimulating the jaw each time we chew.
Oral Health Considerations
Good oral health is essential before we get dental implants. We need healthy gums, since gum disease can lead to implant failure.
Smoking, uncontrolled diabetes, and untreated dental infections can lower our chances of success. Dentists will check for cavities, gum disease, and overall mouth condition.
We can improve our oral health by brushing, flossing, and visiting the dentist for regular check-ups. Treating gum disease or infections before starting implant treatment is very important for long-term results.
Some health conditions—like osteoporosis—can affect candidacy, but with the right care, patients with controlled conditions may still be eligible for dental implants.
Initial Consultation and Treatment Planning
Before choosing dental implants, we need a full assessment from a dental professional. The initial consultation often includes a review of our medical history, dental X-rays, and a physical exam of our mouth and jaw.
The dentist will ask about any medications we take, health problems, and our lifestyle habits, like smoking. Based on this information, the dental team creates a treatment plan.
This plan details the number of implants needed, any steps like bone grafting, the expected timeline, and aftercare. Clear communication during the consultation helps us understand every part of the process, so we know what to expect as we move forward with treatment planning.
Dental Implant Procedure Overview
Dental implants are a reliable way to replace missing teeth. The process involves several important steps, each designed to make sure the implant is secure and long-lasting.
Step-by-Step Implant Process
The dental implant procedure begins with a detailed assessment. We review medical history, take X-rays, and sometimes use 3D scans to check jawbone health.
Planning is crucial, especially if there is not enough bone for the implant, which may mean we need to use bone grafting. Here are the main steps:
- Consultation and Examination: We examine the mouth and discuss the treatment plan.
- Preparation: If a tooth needs extracting or if bone grafting is necessary, we do this first.
- Implant Placement: The titanium post is placed into the jaw.
- Healing: The bone heals and fuses with the implant.
- Abutment and Crown: After healing, we attach the abutment and then the crown.
Every patient’s journey is different and may include extra stages like bone grafts or sinus lifts as appropriate. The full process can take several months, especially if several steps are needed.
Detailed timelines and more information can be found on A Complete guide to Dental Implants Process and Timeline.
Implant Placement
Implant placement is a minor oral surgery performed under local anaesthetic. We make a small incision in the gum to expose the bone.
A precise hole is then drilled into the jawbone for the implant post. The implant is typically made of titanium, which is safe and integrates well with bone.
Once inserted, the gum is closed over the site. Most patients feel only mild discomfort, and normal activities can often be resumed within a day or two.
The procedure to place a single implant usually lasts around one to two hours, but complex cases may take longer. For more details, see Dental Implant Procedure | Timeline, Steps, Recovery & Stages.
Healing Period and Osseointegration
The healing period is a critical stage in the dental implant process. After the implant is placed, we wait for the bone to grow around it.
This process is called osseointegration and usually takes three to six months. During this time, the bone fuses tightly with the titanium post, making the implant secure and stable.
We monitor healing through follow-up visits and X-rays. Good oral hygiene and not smoking help ensure proper healing and reduce the risk of complications.
Once osseointegration is complete, we fit the abutment and crown. This final step restores both function and appearance, giving you a natural-looking tooth that feels strong and comfortable.
Pre-Treatment Considerations
Dental implants need a strong foundation to succeed. Sometimes, we may need to address problems like bone loss or remove damaged teeth before the main procedure.
Bone Grafting
Bone grafting helps us rebuild missing bone in the jaw. If someone has lost teeth for a long time, the bone may shrink or weaken and may not support an implant.
A bone graft can add volume and strength, making the area ready for a secure implant. We use different graft types such as synthetic bone, bone from another part of the body, or donor bone.
Healing time varies and can last several months, but proper healing reduces the risk of implant failure. Signs that bone grafting is needed include severe bone loss seen on X-rays and not enough jaw height or width.
Pain or swelling is common during recovery and we give advice and medicine to manage these symptoms. Careful planning and personalised treatment are key parts of dental implant success.
Tooth Extraction
Sometimes a tooth needs to be removed before placing an implant. This may be due to decay, gum disease, or a broken tooth that cannot be saved.
A clean extraction helps prevent infection and makes space for the implant. We may extract a single tooth or several teeth, depending on the case.
In some situations, a bone graft is placed immediately after extraction to stop bone loss in the area. Healing takes a few weeks to a few months, and we must wait until the gums and bone have healed before starting the implant process.
Key steps include numbing the area, gently removing the tooth, and giving aftercare instructions. We watch for swelling, bleeding, or infection and give clear guidance to speed up recovery.
More details about the implant process and preparation steps can be found here.
Restoring and Completing Dental Implants
Restoring dental implants is a step-by-step process that brings function and a natural look to our smile. The main restoration steps include attaching the abutment and fitting the final crown, which completes the dental work.
Abutment Placement
Abutment placement is the stage when we fit a small metal connector onto the dental implant. This connector links the implant below the gum to the crown above it.
The abutment is usually made of titanium or zirconia, both of which are strong and safe for our mouth. The dentist reopens the gum to place the abutment after checking that the implant has healed and fused to the bone, which often takes a few months.
The gum is then carefully stitched around the abutment, leaving it exposed just above the gumline. The gums need about two weeks to heal.
Proper abutment placement is key. It provides a stable base for the crown and helps keep the restored tooth secure when chewing.
With the abutment in place, we are ready for the final phase of our implant restoration. For more information about the abutment stage, visit this step-by-step guide to dental implants.
Crown Placement and Restoration
Crown placement is the final step in restoring the implant. We start by taking impressions of our mouth so the dental lab can craft a custom crown.
Dentists use strong materials such as porcelain or ceramic to create a lifelike appearance and match the natural shade of our teeth. The crown is securely attached to the abutment using dental cement or a tiny screw.
This method ensures the crown stays in place during everyday use. The dentist will check our bite and make adjustments if needed, so the new tooth feels comfortable and works like a normal tooth.
The restored implant allows us to eat, speak, and smile with confidence. It also helps maintain our jawbone and keep the surrounding teeth stable.
To learn more about dental crown options and what to expect, you can read this dental implant restoration guide.
Tooth Replacement Options Compared
Tooth replacement offers several methods, each with varying levels of stability, comfort, and appearance. The right choice depends on factors like bone health, number of missing teeth, and personal preferences.
Dental Implants vs Traditional Dentures
Dental implants are placed directly into the jawbone, acting as secure anchors for replacement teeth. Traditional dentures, by contrast, sit on top of the gums and are usually removable.
With implants, we maintain jawbone health since the bone is stimulated, helping to avoid bone loss. Dentures can sometimes cause the bone underneath to shrink over time.
Implants feel more like natural teeth and do not slip when we eat or talk. Traditional dentures are an affordable initial option for many people and do not require surgery.
However, their fit can become loose, and they may need adhesive to stay in position. Implants generally last longer and require less maintenance.
They offer better comfort and confidence for daily use. For more details about these differences, see this guide to dental implants.
| Feature | Dental Implants | Traditional Dentures |
|---|---|---|
| Fixed in jawbone | Yes | No |
| Looks/feels natural | Yes | Sometimes |
| Bone preservation | Yes | No |
| Removable | No | Yes |
| Upkeep | Low | High |
Implant-Supported Bridges
An implant-supported bridge involves one or more dental implants placed in the jaw, supporting a bridge of prosthetic teeth. This design can replace several missing teeth in a row without relying on healthy neighbouring teeth for support.
With these bridges, we benefit from added stability. The bridge is fixed and does not shift, which helps with chewing and speaking.
This is a strong choice when multiple teeth are missing in the same area. Implant-supported bridges can help prevent bone loss because implants stimulate the jaw, unlike conventional bridges that depend on natural teeth.
While the initial process takes longer and may cost more, the results are longer lasting and help protect the rest of our teeth from extra wear. Learn more about the advantages of implant-supported bridges.
Removable Dentures
Removable dentures are a widely used tooth replacement option when many or all teeth need replacing. They rest on the gums and are usually made from acrylic.
We can easily take them out for cleaning. These dentures are usually more affordable upfront than implants or fixed bridges.
They are fitted to our mouth and custom-designed for each person. While convenient, they can feel bulky, and some may find it hard to adjust at first.
Removable dentures rely on suction, clasps, or adhesives to stay in place. Over time, bone loss can make them fit less securely, and they might need to be relined or replaced.
Despite these issues, removable dentures remain a practical choice, especially for those with limited bone volume or financial restrictions when compared with other tooth replacement options.
Dental Bridges
A dental bridge is a fixed restoration that uses the natural teeth on either side of a gap to support one or more prosthetic teeth. To place a bridge, we usually need to file down the adjacent healthy teeth so they can anchor the replacement.
Dental bridges restore function for small gaps caused by one or two missing teeth. They are less invasive than implants, but doing so means we alter healthy teeth, which can increase the risk of future dental problems for those teeth.
Bridges are cemented in place, so they do not need removal each night. However, they do not protect against jawbone loss because they do not stimulate the bone like implants do.
Bridges generally need to be replaced every 5-15 years, depending on our oral hygiene and habits. For more on comparing dental bridges to other methods, visit this complete guide on tooth replacement.
Post-Operative Care and Maintenance
Proper post-operative care is necessary for the success of dental implants. Regular cleaning, careful habits, and dentist visits help keep our implants healthy and long-lasting.
Oral Hygiene and Implant Care
We must keep our implants and natural teeth as clean as possible. Using a soft-bristled toothbrush twice daily is recommended.
This helps remove plaque and stops gum inflammation. Flossing is also important to remove food and plaque between teeth and around our implant.
Some dentists suggest using special implant brushes or interdental brushes for improved cleaning. An antibacterial mouthwash may also help lower the risk of infection.
Avoid harsh brushing, as it can damage the gum or implant. We need to limit sugary snacks and drinks, as sugar feeds bacteria and raises the risk of gum disease.
Good oral hygiene habits keep both our implants and natural teeth in good condition.
Routine Check-Ups
Yearly maintenance visits with our dentist are important for checking the health of our implants. These visits include professional cleaning around the implant area and X-rays to look at bone and gum health.
Any signs of infection, inflammation, or movement can be caught early and treated. During routine check-ups, our dentist may give us personalised cleaning tips or new tools to keep our implants clean.
Regular dental care and maintenance help prevent long-term complications and keep our oral health strong. If we notice redness, swelling, or pain around our implants, we should contact our dentist as soon as possible.
Prompt care helps protect our investment and keeps our smiles healthy.
Potential Risks and Complications
Dental implants are usually safe, but certain health problems can raise the risk of complications. Two main risks to watch out for are gum disease and bone loss, which can lead to implant failure.
Gum Disease and Implant Failure
Gum disease, also called peri-implantitis, is a common reason why dental implants fail. Infection happens when bacteria build up around the base of the implant.
This causes gums to become red, swollen, and may bleed easily. If left untreated, it can destroy the tissue and bone that support the implant.
The risk of gum disease increases with poor oral hygiene or if we already have gum problems before getting implants. Smoking and certain health conditions, like diabetes, can also raise the chance of infection.
To lower this risk, it’s important we brush twice daily, floss carefully, and have regular dental check-ups. Warning signs of gum disease include persistent bad breath, pain around the implant, and gums pulling away from the tooth.
Treating these problems early can prevent implant failure. According to WebMD, infection is one of the main complications seen with dental implants.
Bone Loss and Jawbone Issues
Bone loss around implants is another serious problem that can make an implant loose or fail. Our jawbone needs to stay strong to support the new tooth.
However, infection, missing teeth for a long time, or certain conditions can cause the bone to shrink or become too weak to hold the implant. If there is not enough bone, the dentist may need to perform a bone graft before we get the implant.
Even after surgery, ongoing bone loss can still occur if we do not keep the area healthy. People with osteoporosis or who take certain medicines may have a higher risk.
Jawbone issues can also cause implants to press into nearby areas, such as the sinuses when implants are placed in the upper jaw. Tooth implants must be placed carefully to avoid damage and make sure the bone stays healthy.
Regular checks let us find and treat bone loss early.
Cost, Insurance, and Financing
Understanding the price of dental implants, what type of dental insurance may help, and available financing options can help us make informed decisions. There are many factors that affect the total cost, and different ways to manage the expense if we need help paying for treatment.
Factors Affecting Price
Several factors influence dental implant costs. The price per tooth usually ranges from £1,795 to £4,500 in the UK for 2025, depending on the clinic’s location, the dentist’s experience, and the materials used.
For complex cases, such as when we need bone grafting or sinus lifts, the cost can be higher. A full mouth of implants is much more expensive.
The price may range from £20,000 to £45,000 based on the extent of work required, but some clinics offer options from around £15,995 for full-mouth restoration. It’s important to know that the final bill is not just for the implant itself.
We should also consider consultation, scans, surgery, and follow-up appointments. Regional differences are another key aspect.
Clinics in London and major cities often have higher fees compared to other areas. To see a detailed breakdown, we can review this comprehensive price guide for dental implants in London.
Dental Insurance Coverage
Most standard dental insurance does not cover the full cost of dental implants. In the UK, both NHS and private dental insurance typically focus more on preventive and restorative treatments like crowns, fillings, and extractions.
Implants are often considered a cosmetic procedure. Some private dental insurance plans may help with part of the bill.
These plans might cover the crown that goes on top of the implant or provide a small set benefit towards implant surgery. It is important for us to check the policy details and ask our provider if major procedures like implants are included.
We should also be aware of annual limits and waiting periods. Even with extra cover, insurance rarely pays for the whole process.
We need to budget for the out-of-pocket part, which can be significant.
Financing and Payment Plans
Dental clinics often offer financing or monthly payment plans to make implant treatment more accessible. These plans let us spread the cost over 1 to 5 years, which can reduce the pressure of paying everything upfront.
Some clinics partner with finance companies to offer interest-free or low-interest loans for dental work, sometimes for up to 12 or 24 months. This can be a good option for people without insurance or when insurance does not cover implants.
It is important for us to look at the terms and conditions, such as the interest rate, repayment schedule, and any early repayment fees. This helps us understand the total amount we will pay over time.
Many patients find it helpful to compare financing options across clinics to get the best terms for their situation.
Choosing a Dental Implant Provider
Selecting the right dental implant provider can make a big difference in the success and safety of our treatment. We need to pay attention to the dentist’s qualifications and experience, as well as practical factors like location, especially when looking for care in places such as Leicester.
Qualifications and Experience
We should always check a provider’s training and background before scheduling a dental implant procedure. Dentists who place implants must have not only a dental degree but also extra education in implant dentistry.
In some areas, dentists are required to complete additional hours of education specifically in dental implants. For example, in certain regions, dentists need at least 56 hours of extra study before they can place implants.
It’s important to choose providers with a proven record in oral surgery. We can ask about the number of implant procedures they have performed and their success rates.
Providers who use modern technology and stay updated through ongoing training are more likely to deliver safe and reliable results. Comparing a few clinics in our area helps us find someone who combines both skill and up-to-date techniques, increasing our confidence in the provider’s ability to handle complex cases.
We can also read more about what to look for in an implant provider at this complete guide to dental implant qualifications.
Location Considerations: leicester
When searching for a dental implant provider in Leicester, convenience and accessibility are key. We want a clinic that is easy to reach from our home or workplace, with flexible appointment times to fit our schedules.
Local providers are also helpful if we need urgent care or follow-up visits. It helps to research clinics that specialise in dental implants and oral surgery within Leicester.
We can compare their services, technologies, and pricing. Getting recommendations from friends and reading online reviews can give us insight into the clinic’s reputation and patient satisfaction.
Some Leicester clinics may offer free initial consultations, allowing us to meet the team and discuss our treatment options before deciding.
Frequently Asked Questions
We often receive questions about dental implants, including their procedures, costs, types, and recovery experiences. Understanding these topics can help us make informed decisions about dental care and what to expect at each stage.
What are the steps involved in a full mouth dental implant procedure?
A full mouth dental implant procedure usually starts with an assessment and treatment plan. This involves dental scans and X-rays to check our bone health and oral condition.
If jawbone strength is not enough, bone grafting may be needed before placing implants. We receive the implants surgically, followed by a healing period before attaching the final crowns or dentures.
How much do different types of dental implants typically cost?
The cost of dental implants can vary based on the number of implants, the type of material, and the dentist’s location. Single implants tend to cost less than full mouth implants or bridges.
For a single tooth implant, the price in the UK can range from £2,000 to £2,500. Full mouth dental implants can cost much more and will depend on our individual needs.
Some clinics share more details about typical costs.
What are the most common types of dental implants available?
The two main types of dental implants are endosteal and subperiosteal implants. Endosteal implants are most common and are placed directly in the jawbone.
Subperiosteal implants are positioned on top of the jawbone but under the gum. We may also hear about mini implants and zygomatic implants, which are specially designed for unique dental needs or less bone.
What potential side effects should one be aware of following a tooth implant?
Side effects after a tooth implant include swelling, bruising, minor bleeding, and discomfort near the site. These are normal and usually fade within days.
There is also a small risk of infection or implant failure. Following our dentist’s advice and maintaining good oral hygiene reduces these risks.
Smoking can increase the chance of problems with healing.
What is the typical timeline from tooth extraction to completing an implant?
If an extraction is needed, healing time before an implant can range from a few weeks to a few months. The jawbone needs to recover before the implant is placed.
The implant itself is then inserted and needs more time, usually three to six months, for the bone and implant to fuse. After that, the permanent crown or bridge is attached.
Each person’s timeline may differ based on their healing and treatment needs.
Can I view a detailed, step-by-step breakdown of the dental implant process?
Yes, clinics often share a complete walkthrough of the dental implant process, from first consultation to the final fitting of the replacement tooth.
This includes pre-surgery imaging, anaesthesia, implant placement, healing, and fitting the final crown.
We can explore a detailed explanation of each step online to better understand what will happen at every stage of our dental implant journey.






